Combination therapy with vitamin A is safe for pancreatic cancer patients, trial shows
A treatment combining a form of vitamin A with the current standard treatment for pancreatic cancer is safe for patients, according to an early phase clinical trial led by Barts Health consultant Professor Hemant Kocher.
Following the encouraging results of this phase I trial (STARPAC), published today in Nature Communications, a second clinical trial called STARPAC2 will now investigate whether the addition of this form of vitamin A, called ATRA, to standard chemotherapy can enhance the efficacy of treatment in patients with pancreatic cancer.
STARPAC was launched following research conducted by Professor Kocher’s laboratory, which found that treating a particular type of cell, known as stellate cells, within pancreatic tumours with ATRA restricted tumour growth.
Stellate cells have an important role in normal tissue formation, however, they become corrupted in cancer and help to form an impenetrable barrier, known as the stroma, around the pancreatic tumour.
Treating stellate cells with ATRA (a pre-existing drug used for the treatment of acne and some types of leukaemia) was found to restore the vitamin A content of the cells, converting them from tumour-promoting cells to cells which have an anti-cancer effect.
By combining this drug with chemotherapy in preclinical models, the team were able to disrupt the communication between the cancer cells and the surrounding stromal cells, leading to a reduction in cancer cell proliferation and invasion.
To determine the safety of this treatment combination in the clinic, patients were recruited to the phase I STARPAC trial from a number of trusts including Barts Health NHS Trust.
The trial showed that the addition of ATRA to standard chemotherapy had no additional harmful effects in patients when compared with the standard chemotherapy alone, and also demonstrated that the combination does seem to modify the pancreatic cancer stroma in patients.
'Exciting discovery'
 Hemant Kocher, consultant liver and pancreas surgeon at Barts Health NHS Trust and professor at Queen Mary University of London's Barts Cancer Institute said: “It's pleasing to demonstrate that changes in the stroma (or scar tissue) surrounding cancer can be used to potentially change pancreatic cancer behaviour.
Hemant Kocher, consultant liver and pancreas surgeon at Barts Health NHS Trust and professor at Queen Mary University of London's Barts Cancer Institute said: “It's pleasing to demonstrate that changes in the stroma (or scar tissue) surrounding cancer can be used to potentially change pancreatic cancer behaviour.
"This proof-of-principle that the stroma can be targeted in patients is a novel and exciting discovery, and this approach may also be able to be applied to other cancers and diseases where the stroma performs a critical role in disease progression.”
The trial was performed in collaboration with the Institute of Cancer Research, London and the Cancer Research UK Cambridge Institute, and funded by the Medical Research Council (MRC) with support from Celgene Corporation.
Following on from STARPAC, the MRC is to award £1.5million to fund a phase II clinical trial that will set out to determine whether the addition of ATRA to current standard chemotherapy can improve the treatment outcome in pancreatic cancer.
The MRC grant will be accompanied by approximately £1million worth of ‘drugs in kind’ provided by Celgene.
Lowest survival rate
There are around 10,300 new pancreatic cancer cases diagnosed in the UK each year and, although this accounts for only 3% of the total cancer cases, pancreatic cancer has the lowest survival rate of all common cancers.
It claims the lives of approximately 9,200 people each year and only around 7% of those diagnosed survive for five years or more.
Chemotherapy and radiotherapy alone are relatively unsuccessful in treating pancreatic cancer, and while surgery to remove the tumour offers the best chance of survival, a lack of symptoms in the early stages of the disease means most patients are diagnosed when the cancer is advanced.
A novel approach that is able to target the cancer more effectively is therefore urgently required.
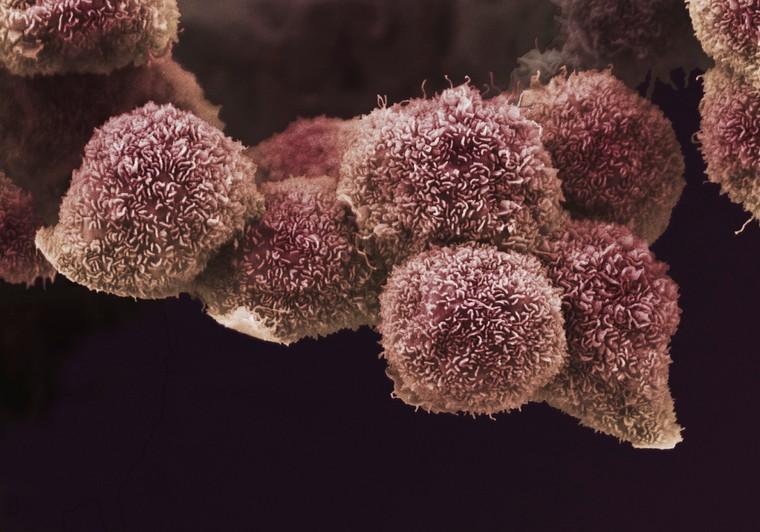
Picture credit: Anne Weston, Francis Crick Institute. Attribution-NonCommercial 4.0 International (CC BY-NC 4.0)
Read more
 Afrikaans
Afrikaans Albanian
Albanian Amharic
Amharic Arabic
Arabic Armenian
Armenian Azerbaijani
Azerbaijani Basque
Basque Belarusian
Belarusian Bengali
Bengali Bosnian
Bosnian Bulgarian
Bulgarian Catalan
Catalan Cebuano
Cebuano Chichewa
Chichewa Chinese (Simplified)
Chinese (Simplified) Chinese (Traditional)
Chinese (Traditional) Corsican
Corsican Croatian
Croatian Czech
Czech Danish
Danish Dutch
Dutch English
English Esperanto
Esperanto Estonian
Estonian Filipino
Filipino Finnish
Finnish French
French Frisian
Frisian Galician
Galician Georgian
Georgian German
German Greek
Greek Gujarati
Gujarati Haitian Creole
Haitian Creole Hausa
Hausa Hawaiian
Hawaiian Hebrew
Hebrew Hindi
Hindi Hmong
Hmong Hungarian
Hungarian Icelandic
Icelandic Igbo
Igbo Indonesian
Indonesian Irish
Irish Italian
Italian Japanese
Japanese Javanese
Javanese Kannada
Kannada Kazakh
Kazakh Khmer
Khmer Korean
Korean Kurdish (Kurmanji)
Kurdish (Kurmanji) Kyrgyz
Kyrgyz Lao
Lao Latin
Latin Latvian
Latvian Lithuanian
Lithuanian Luxembourgish
Luxembourgish Macedonian
Macedonian Malagasy
Malagasy Malay
Malay Malayalam
Malayalam Maltese
Maltese Maori
Maori Marathi
Marathi Mongolian
Mongolian Myanmar (Burmese)
Myanmar (Burmese) Nepali
Nepali Norwegian
Norwegian Pashto
Pashto Persian
Persian Polish
Polish Portuguese
Portuguese Punjabi
Punjabi Romanian
Romanian Russian
Russian Samoan
Samoan Scottish Gaelic
Scottish Gaelic Serbian
Serbian Sesotho
Sesotho Shona
Shona Sindhi
Sindhi Sinhala
Sinhala Slovak
Slovak Slovenian
Slovenian Somali
Somali Spanish
Spanish Sundanese
Sundanese Swahili
Swahili Swedish
Swedish Tajik
Tajik Tamil
Tamil Telugu
Telugu Thai
Thai Turkish
Turkish Ukrainian
Ukrainian Urdu
Urdu Uzbek
Uzbek Vietnamese
Vietnamese Welsh
Welsh Xhosa
Xhosa Yiddish
Yiddish Yoruba
Yoruba Zulu
Zulu